New system for detecting Parkinson’s early
Parkinson’s disease is a debilitating neurodegenerative disease, affecting everything from speech, posture and gait to digestion, sleep, impulse control and cognition. Therapies exist that alleviate some symptoms of the disease, but there is still no cure for Parkinson’s, which affects close to one million Americans and 10 million people worldwide.
A new Tel Aviv University study unveils a novel method for detecting the aggregation of the protein alpha-synuclein, a hallmark of Parkinson’s disease. With this knowledge, caregivers could introduce treatment that has the potential to significantly delay disease progression.
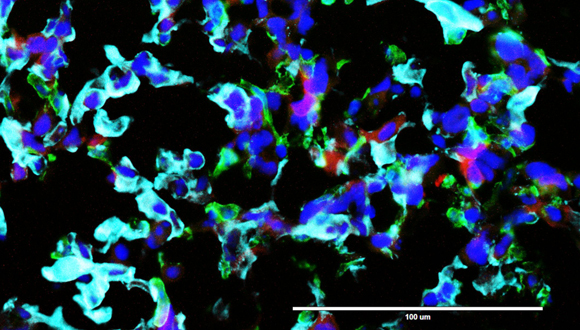
By the time a patient is diagnosed with Parkinson’s disease, 50 percent to 80 percent of the dopaminergic cells in the part of the brain called substania nigra are already dead, possibly due to development of toxicity as result of alpha-synuclein aggregation. “We have developed a new method for tracking early stages of aggregation of alpha-synuclein using super-resolution microscopy and advanced analysis,” says Prof. Uri Ashery, co-author of the study and head of TAU’s Sagol School of Neuroscience and TAU’s George S. Wise Faculty of Life Sciences. The research was published in Acta Neuropathologica on May 31.
“Together with our collaborators at Cambridge University, who developed a special mouse model for Parkinson’s disease, we were able to detect different stages of the aggregation of this protein,” Prof. Ashery explains. “We correlated the aggregation with the deteriorating loss of neuronal activity and deficits in the behavior of the mice.”
A big step towards early detection
“This is extremely important because we can now detect early stages of alpha-synuclein aggregation and monitor the effects of drugs on this aggregation,” says Dr. Dana Bar-On of the Sagol School of Neuroscience, a co-author of the study. “We hope that this research can be implemented for use in the early diagnosis of Parkinson’s in patients. We’re currently working to implement the methods in a minimally invasive manner with Parkinson’s patients.”
The researchers, in collaboration with the Max Planck Institute in Gottingen and Ludwig-Maximilians-Universität München, were able to illustrate the effect of a specific drug, anle138b, on this protein aggregation and correlated these results with the normalization of the Parkinson’s phenotype in the mice, according to Prof. Ashery. “This is a significant step forward in the world of Parkinson’s research,” he says.
The researchers are planning to expand their research to family members of Parkinson’s disease patients. “By detecting aggregates using minimally invasive methods in relatives of Parkinson’s disease patients, we can provide early detection and intervention and the opportunity to track and treat the disease before symptoms are even detected,” Prof. Ashery concludes.